Ankle Replacement


This operation replaces the degenerate joint with metal and polyethylene.
It is similar to a knee replacement. The surfaces of the joint are replaced with specially designed metal replacements, which articulate with a very strong plastic insert (ultra-high density polyethylene).
Once healed, the joint will be mobile and ideally pain free, although some discomfort should be expected.
Following surgery, you should be able to walk much more normally, with minimal pain and often with more movement than before.
Although joint replacements in the hip and knee have been studied for decades now, Ankle replacements are relatively new and do not have such long term information on outcome. Currently we have results on the survival (success) for 10-12 years with approximately 90% of operations remaining a success – this is similar to the success rates for knee replacement.

The ankle joint is made up of the Tibia articulating with the talus...

Ankle arthritis occurs when the cartilage of the joint has worn out and degenerated, so that the joint articulation is now bone rubbing on bone (loss of joint space on xray). This causes the bone to become thicker and sclerotic (whiter on xray) and to form large spurs around the periphery of the joint (osteophytes).
Vantage® Total Ankle System
I use the Vantage Total Ankle Replacement.
Through the collaboration and innovation of engineering and surgeon thought leader expertise, the Vantage Ankle achieves a new perspective in total ankle by addressing clinical challenges and patient outcomes. Our proprietary CT reconstruction studies evaluated both healthy and diseased ankles to shape our curved and flat cut taluses and tibia components.

This combines the latest technological advances with the proven designs and methods, from over the last 30 years.
The steel components have a plasma sprayed titanium backing that bone grows into, securing the impants for the long term. The articulation is using ultra high molecular weight polyethylene which has a proven track record in hip and knee replacements for the last 3 decades.
Recent Studies have shown reliable long term results for Ankle Replacement with good survival rates for at least 10 years (there are no studies with results longer than this yet). In my own series of patients for over 18 years, we have had excellent results. Of Course, it doesn’t work for everybody but the failure rates are low and equivalent to that of ankle fusion.
Latest Results 2024:
Ankle arthrodesis or total ankle arthroplasty surgery for end stage ankle arthritis, which is best? A review of the best available evidence.
Foot Ankle Surg. 2024 Glazebrook et al
There is fair evidence that supports both Total Ankle Replacement TAA and Ankle Fusion AA for the surgical treatment of End stage Ankle Arthritis. However, TAA trended to be superior for pain relief, activity, health related quality of life and readmission rate, while AA trended to be superior for revision rates).
Preparation for Surgery
You should have received a letter detailing the codes and costs for the surgery and giving instructions on where to go and at what time. Please check these details carefully as you will be liable for any costs not covered by your insurers.
You will need to be nil-by-mouth – No food for 6 hours before surgery. Clear fluids can be taken for up to 2 hours before the operation.
MRSA status
Before or on admission to hospital a nasal swab will be taken to screen for MRSA. There is a small chance this is positive. If so your operation will be moved to the end of the list or rarely to another day to prevent cross infection.
Prior to surgery
It is important to prepare for the forthcoming surgery.
a) Leg care - make sure that the leg and skin are as healthy as possible.
- The surgery cannot go ahead if there are any grazes, insect bites or infections. Please notify Fortius if you have any of these.
- If you suffer from swollen ankles, use a compression sock or keep the legs elevated as much as possible for 1-2 days before surgery.
b) Prepare for non-weightbearing as you cannot walk on the leg for the first 2 weeks!
- This has so much value. Ideally see a physiotherapist to teach you how to use crutches, or if that is not possible to use a frame.
- There are other devices that can really help.

The knee rover is a scooter with brakes that takes the weight of the leg. www.kneerover.com

The iWalk is a ‘peg-leg’ – it requires good balance.
c) Prepare your stay at home.
- How to elevate the leg – the ankle will need to be up high above the knee and hip for 2 weeks. Either in bed or on the Sofa 45mins per hour. You cannot sit in a chair for more than 1-2 mins.
- Food requirements
- Washing & Bathing – you will be given a waterproof cover. Using a cheap plastic chair in the shower will make it much easier.
- Managing stairs. Depending on your competence on crutches, you may want to move a bedroom downstairs so everything is on one floor.
- Assistance at home – there are plenty of private nursing services that can help.
- Post operative hotels – it may be easier to check in for a 2 week stay. This is not usually covered by your insurers.
d) On the day of surgery.
- No food, drink or smoking 6 hours before surgery (clear water can be taken up to 2 hours before)
- Please bring any xrays and scans of the ankle with you
Admission
You will need to go to hospital at least 2 hours prior to the surgery, to prepare for surgery and for your stay at hospital. The surgery can be performed as a day case, but most patients stay 1 night. Your length of stay in hospital will depend on your ability to get up on crutches or a frame, so time spent in training prior to surgery will be valuable.
Surgery
The surgery takes about 2 hours to perform depending on the complexity. It is usually performed under general anaesthetic with a "popliteal block" – this is the same as an epidural but placed at the knee. It will make your leg numb below the knee for 1-3 days and provides excellent pain relief.
The surgery is performed through a 15cm incision over the front of the ankle. The ankle joint is carefully exposed, taking great care to protect the nearby nerves and arteries. Using precise cutting jigs and xray guidance, the arthritic joint surfaces are excised (cut out) and the tibia and talus shaped to receive the new joint. A trial or practice implant is then used to check the final surgery, positioning and flexibility are correct.
The ankle replacement implants are then inserted locked in place. They implants are “uncemented” – they have a special titanium plasma sprayed coating that bone grows into, securing them in place for years
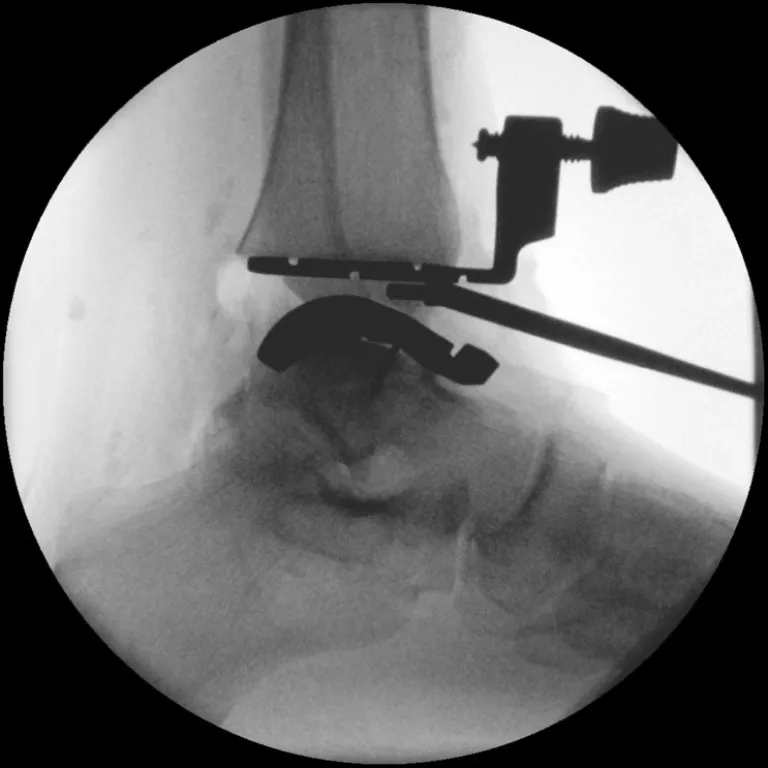
Intra operative xrays
Using the latest and best techniques, with precision implants and guides for exact placement and alignment of TAR. Throughout surgery, the alignment and positioning is continually checked using xrays and the custom built guides for insertion for precise resection of the arthritic joint surfaces and the best possible ankle joint replacement.

Final images
The precise alignment jigs allow for exact placement of the ankle joint at the centre of the mechanical axis. This is one of the variables that ensure best function of the ankle and long term survival.
At the end of surgery, your leg will be immobilised in a backslab (half plaster) for 2 weeks.
Post Surgery
Elevation of the foot (above the pelvis) for the first 10 days is vitally important to prevent infection. Sitting in a chair is not possible for more than a few minutes, and you will need to be reclining in bed or on the sofa.
Naturally, small periods of walking and standing are necessary, but no weight must be taken through this leg for 2 weeks.
After 2 weeks the backslab will be removed and the stitches taken out, here in clinic. If all is well, you can begin weight bearing at that stage. Physiotherapy to regain the ankle motion, can start at this stage.
"I would like to thank you for the wonderful job done... a huge success. I walk my dogs over rough ground, climb up fairly steep slopes with little or no swelling. In short I am thrilled with the operation!".
LW

New ankle replacement reaches of top of mountain in Mongolia!
Risks of surgery
Swelling
Initially the foot will be very swollen and needs elevating. The swelling will disperse over the following weeks & months but will still be apparent at 6-9 months.
Infection
This is the biggest risk with this type of surgery. Smoking increases dramatically. You will be given intravenous antibiotics to prevent against it. The best way to reduce your chances of acquiring an infection is to keep the foot elevated for 10 days. If there is an infection, it is usually mild and resolves with a course of antibiotics. Rarely, it can be severe requiring further surgery.
Nerve Damage
Alongside the incision are three nerves – the deep & superficial peroneal and the saphenous nerves. They supply sensation to the side and the top of the foot and toes. They may become damaged during the surgery and this will leave a patch of numbness, either at the side of the foot or over the top of the foot and toes. This is usually temporary but may be permanent. There is approximately a 10% of this happening.
Wear of the replacement
The metal / polyethylene joint has an unknown lifespan at present. When it fails, it is either due to infection or wearing away of the polyethylene. This usually takes several years; we do not have an average longevity yet. Once the joint wears out, further surgery is normally required to fuse the joint together. Hopefully, this never becomes necessary, but a 10-15 year period is a reasonable estimate for the survival of the ankle joint.
Blood Clots
There is a risk of DVT until you are walking on the ankle. You will be given protective calf pumps during surgery and anticoagulants post operatively, to reduce this risk. Despite this there is still a small chance one occurs. If this happens you will treated with further tablets.
Fracture
There is a risk in up to 10% of cases. The surgery is performed through a very tight space to access the ankle joint, unlike other joints where the entire joint can be exposed. Occasionally one of the side bones of the ankle joint fractures during the surgery - If this happens it will be fixed immediately.
Dislocation
This is rare.
Immediately after surgery
You will be referred to a physiotherapist who will advise on walking while keeping weight off the ankle using crutches. You will be sent home only when you are comfortable.
Pain relief and take home medications
You will be given high doses of prescription painkillers to take home. Use these for the first 2-3 days and reassess.
There is a small risk of blood clots “DVT’s” with Achilles surgery and you will be prescribed a blood thinner for 2 weeks.
Recovery from surgery
This is significant surgery and patience will be required in a aiding a gradual recovery process. Strict elevation for many days after the procedure is necessary to control swelling and improve wound healing.
- Expect swelling for over one year! A long compression sock can help with this.
- Expect discomfort for 6 months.
- Driving should be possible after 4-6 weeks.
- It will take 4-6 months for you to be able to walk for over ½ hour.
Activity and time off work
- In general, 4 weeks off work is required for sedentary posts
- 8 weeks for standing or walking posts
- If you are a farmer, gardener or involved in similar active pursuits it may be 12 weeks before you can begin to put strain on the joint.
Follow up
- 2 weeks for removal of sutures & plaster
- 6 weeks in Mr Rosenfeld's clinic: AP & Lateral X-rays
- 3 Months: WB X-ray
- 6 months: WB X-ray and Annual X-rays thereafter.
Faqs
Manual - When you can do an emergency stop safely no earlier than 4 weeks
Automatic - With left leg week 2
Sedentary – 2 weeks WFH and week 4 return to office
Standing – 6 weeks
Manual labour – 12-16 weeks return to work
6 weeks post op can safely bike outdoors
12-16 weeks post op with supervision of this milestone with Physio
Once wounds are dry and mature – usually 3-4 weeks
4-6 months post to discuss milestone with physio
Week 6 onwards although it may take longer due to swelling
6 months post discuss with physio and consultant