Distal Tibial Realignment Osteotomy
Shifting weight away from the damaged part of the ankle joint
What is it?
This operation is used as a delaying procedure for a specific type of ankle arthritis - when the arthritis has worn primarily on one side of the joint, leaving potentially healthy cartilage on the unaffected part – “varus” or “valgus” ankle arthritis.
It can delay the next stage for several years – and postpone an ankle fusion or an ankle replacement. In the fortunate few it may be the only operation needed.

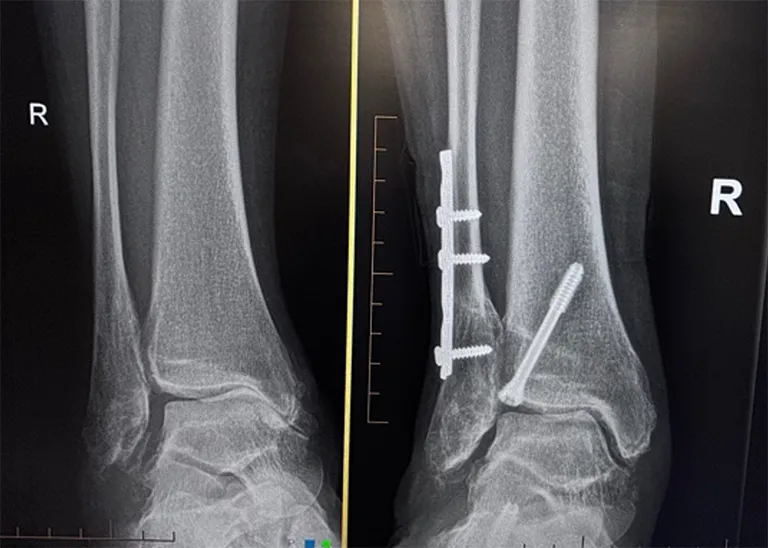
Varus ankle arthritis with bone on bone contact on the medial / inner aspect of the ankle.
The goal is to offload the worn area and redistribute weight to the healthier cartilage on the opposite side of the ankle.
This is achieved by realigning the ankle joint by cutting the tibia (osteotomy) and either removing or adding a wedge on one side, to realign the tibia and ankle. Removing a wedge is called a “closing wedge” osteotomy and adding a wedge an “opening wedge” osteotomy. Often the fibula needs cutting and realigning too. The fibula and tibia are then fixed with plates and / or screws.
I prefer to perform this “minimally invasively” which minimises the damage to the tissues, the complications and improves healing. ( MIDTO – Minimally invasive distal tibial osteotomy).
48 yr old female, 3 years after distal tibia & calcaneal osteotomies performed percutaneously using minimally invasive techniques
Often the realignment is augmented with a calcaneal osteotomy - cutting and shifting the heel bone. This is done at the same time to help fully correct the overall alignment. Again I use minimally invasive surgery for this part of the operation which is fixed with a headless compression screw. (MICO – Minimally Invasive Calcaneal Osteotomy).
Best Suited For:
- Early or asymmetric ankle arthritis
- Younger or active individuals who want to delay fusion or replacement
- Good remaining cartilage in at least part of the joint

Results of surgery
The short to mid-term results of this type of surgery are very good and the majority of patients get excellent relief for many years. It may be better to consider this as an interim procedure, as the underlying arthritis will continue to affect the joint and so symptoms can often recur after several years.
Supramalleolar osteotomy for the treatment of ankle osteoarthritis leads to favourable outcomes and low complication rates at mid-term follow-up: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023
Surgery
The surgery takes about 2 hours to perform depending on the complexity. It is usually performed under general anaesthetic with a "popliteal block" – this is the same as an epidural but placed at the knee. It will make your leg numb below the knee for 1-3 days and provides excellent pain relief.
The surgery is performed through keyhole incisions on one side of the ankle, depending on the type of correction required. The tibia is cut using specialised minimally invasive instruments. Often the fibula is cut too.
The surgery is performed using intra operative xrays. Once the right amount of bone has been removed or realigned, this is assessed with xrays and clinical alignment, the osteotomy / bones are then securely fixed with screws or plates.
The incisions are carefully closed and the leg then immobilised in a temporary cast or “backslab”.
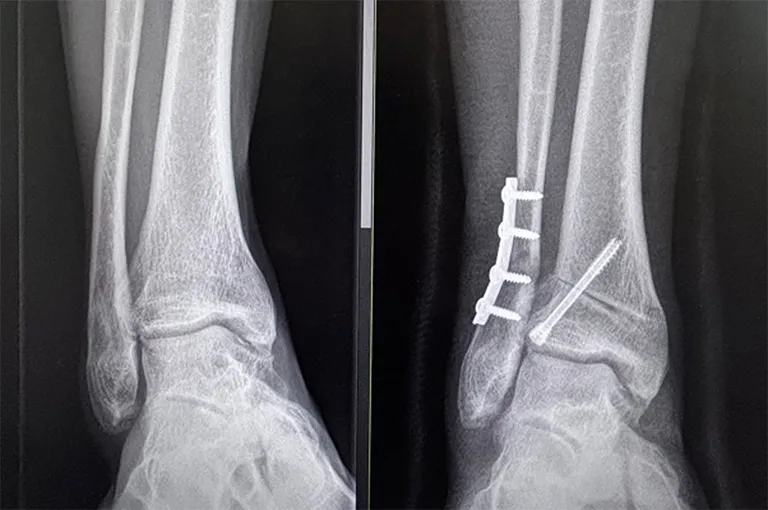
48 yr old female, 3 years after distal tibia & calcaneal osteotomies performed percutaneously using minimally invasive techniques
Immediately after surgery
After surgery, your leg will be immobilised in a backslab (half plaster) for 2 weeks. Elevation of the foot (above the pelvis) for the first 2 weeks is vitally important to prevent infection. Naturally, small periods of walking and standing are necessary, but no weight must be taken through this leg for 4 weeks.
You will be seen by a physiotherapist on the ward, who will advise on using crutches and your rehabilitation. You will be allowed home only when you are comfortable and capable.
Weight-bearing
You cannot walk on the foot for 4 weeks. Initially you will be an plaster cast for 2 weeks and then a protective boot for 6-8 weeks. Walking can start at the 4 week stage, in the protective boot. It will take another 4-6 weeks to be able to walk without the boot and several months to walk normally.
Using crutches can be difficult even for the able-bodied. There are some useful aids that can be bought or hired.

The knee rover is a knee-scooter with brakes that takes the weight of the leg.
The iWalk is a ‘peg-leg’ – it requires good balance.
Risks of surgery
Swelling
Initially the foot will be very swollen and needs elevating. The swelling will disperse over the following weeks & months but will still be apparent at 9-12 months.
Infection
This is the biggest risk with this type of surgery. You will be given intravenous antibiotics to prevent against it. The best way to reduce your chances of acquiring an infection is to keep the foot elevated for 2 weeks. If there is an infection, it should resolve with a course of oral antibiotics. Very rarely a severe infection occurs, requiring IV antibiotics as an inpatient.
Nerve Damage
Alongside the incisions there are small cutaneous nerves. They may become damaged during the surgery - this will leave a patch of numbness at the sides or on top of the foot. This numbness may be temporary or permanent. There is approximately a 5% risk of this happening.
Failure to relieve all symptoms
The results from this surgery are good. Published studies show significant improvement in pain levels that last for more than 5 years in the majority of cases.
Continued Arthritic Pain
The joint will still have arthritic damage and this may continue to progress, at varying speeds. Rarely, realigning the joint can even make these worse requiring further surgery.
Delayed bone healing or Non-Union
The osteotomy normally heals very quickly, but occasionally this can be slow and take several months longer. Rarely, it may not heal at all requiring further surgery. (Especially in smokers, heavy drinkers and diabetics).
Blood Clots
There is a small risk of developing a DVT and to help prevent this you will be prescribed a daily anticoagulant to take until walking.
Preparation for Surgery
You should have received a letter detailing the codes and costs for the surgery and giving instructions on where to go and at what time. Please check these details carefully as you will be liable for any costs not covered by your insurers.
You will need to be nil-by-mouth – No food for 6 hours before surgery. Clear fluids can be taken for up to 2 hours before the operation.
This operation normally requires an overnight stay of 1-2 days.
MRSA status
Before or on admission to hospital a nasal swab will be taken to screen for MRSA. There is a small chance this is positive. If so your operation will be moved to the end of the list or rarely to another day to prevent cross infection.
Anticoagulants
If you are taking an anticoagulant, this will need to be stopped / changed prior to the surgery. Please discuss this with the specialist that prescribed it. Your surgery cannot go ahead without this.
Anaesthetic
The surgery is performed under a general anaesthetic. On top of this you will be given a regional block - an epidural of the leg which numbs the leg for 1-3 days, providing excellent pain relief.
Recovery from surgery
Please make an appointment for a review at 2 weeks, when the backslab will be removed and the stitches taken out. The plaster cast is changed for a protective boot at that stage and physiotherapy can start. Partial weightbearing can start at the 4 week stage. You will be reviewed again at the 6 week stage, when you can start fully walking in the protective boot which will need to be worn for a further 4-6 weeks.
You will be reviewed again at 3 months following surgery, with x-rays.
Physiotherapy is an essential part of your recovery and will start at 2 weeks. Naturally you will get stronger each week but it will take many months to regain full activity.
Pain relief and take home medications
You will be given high doses of prescription painkillers to take home. Use these for the first 3-4 days and reassess.
Washing and Bathing
It’s important to keep the dressing completely dry – the nurses will show you how to do this with a waterproof cover.
Activity and time off work
In general, up to 4 weeks off work is required for sedentary posts. 12 weeks for standing or walking posts. 16 weeks for manual / labour intensive posts.
When can I start to drive again?
The DVLA states that it’s the responsibility of the driver to ensure they are always in control of the vehicle. With surgery to the left leg, driving an automatic is permitted after 2 weeks. On the right leg, driving will not be possible until 6-8 weeks.
It remains your responsibility to drive safely and you should also check with your vehicle insurer to confirm you are covered.